An efficient and easy to use screening kit for cervical cancer: A need of the hour

Cervical cancer is cancer of the cells in the cervix. It occurs when cervix cells start to transform into precancerous cells. It is the fourth most frequent female malignancy, which accounted for more than 600,000 new cases and 342 thousand deaths globally in 2020 (GLOBOCAN), making it one of the top global health issues. Almost 90% of these deaths took place in low- and middle-income nations, where screening and treatment are often limited or inaccessible. In Indian women, it is the third most common cancer and more than 450 million women aged 15 years and above are at risk of developing this cancer.
Dr. Savita Yadav, Professor
Department of Biophysics,
All India Institute of Medical Sciences
New Delhi-110029
The majority of cervical cancer cases are associated with high-risk human papillomavirus (HPV) infections. HPV is an extremely common virus, which is usually transmitted through sexual contact. Among the high-risk strains, HPV types 16 and 18 are the most common. The risk factors of cervical cancer are thus predominantly associated with acquiring HPV infection, impaired immune response to HPV infection, or both. The risk of HPV infection increases by an early age of sex debut, multiple sex partners, giving many births, using oral contraceptives for more than five years, immunosuppression, and smoking. Thankfully, there is a vaccine that can offer defence against some of the most harmful HPV strains. Depending on the recipient’s age, the HPV vaccine is commonly administered in two or three doses. It is advised for adolescents between the ages of 11 and 12 since the HPV vaccine is most effective when administered to people before they become sexually active. However, the vaccine can still be effective for those who have already become sexually active, as long as they have not been exposed to the strains of HPV.
Cancer treatment plans are highly focused and precisely aided by multiple diagnostic tests, such as CT scans, ultrasound, MRI, and biopsy along with physical examination used for detection and monitoring of the disease. Because of the high prevalence rate, women between the ages of 25 and 65 are frequently screened for cervical cancer through cytological screening-Pap smear test. In this test, cells from a woman’s cervix are collected and examined for any anomalies or early cancer indications. In case of abnormal Pap results, further testing is required, which can involve an HPV test, a specialised test that detects HPV infection in the cells of cervix. If a doctor suspects cancer, he might additionally check cervix and requests a tissue biopsy for confirmation.
Cervical cancer is curable if detected in the early stages and treated promptly. Depending on the stage of the malignancy, the survival rate varies widely. If diagnosed in early stages (I or II), the 5-year survival is substantially higher (50-90%), which drops to only 15–35% if diagnosed in an advanced stage (III and IV). Education and access to preventative measures are key to reducing the incidence and mortality rates of cervical cancer worldwide. Fortunately, it is highly preventable with proper screening and vaccination. Regular Pap smear and HPV tests can detect abnormal cells before they turn into cancer, and the vaccine can protect against some of the most dangerous strains of the HPV. However, these current screening methods have some limitations. These tests are expensive and necessitate sophisticated infrastructure and qualified personnel. Also, a conservative outlook of our society towards sexual health denies millions of women basic reproductive health rights. This increases incidence of cervical cancer by preventing its early detection via the conventional screening procedures due to mental barrier of patients regarding their privacy. Other factors like low awareness and lack of skilled personnel also impede the full implementation of these screening tests.
Our research team at the All Institute of Medical Sciences, New Delhi is working in this direction with the ultimate goal of providing the rural, underprivileged and remote population of India with an easy-to-use commercially available screening kit, which will empower them in the fight against cervical cancer. In order to identify cervical cancer biomarkers that can be utilized to develop a screening method/ kit for early diagnosis of cervical cancer, we are investigating alterations in saliva proteins using high throughput mass spectrometric techniques. Once deemed merely a digestive juice, saliva is now being considered a biological fluid capable of communicating an individual’s current health status and we have preferably chosen saliva over blood because its collection is skill-undemanding, non-invasive, and painless. Moreover, saliva samples are safer to handle, easier to collect, ship and store.
Conclusively, despite the fact that significant advances are being made in the field, we require improved diagnosis and prevention strategies to reduce the burden of cervical cancer. The incidence rate can be significantly reduced by a screening or detection method that removes constraints imposed by infrastructure, qualified staff, and hesitation. Moreover, awareness campaigns emphasizing the need of routine cervical cancer screening and HPV vaccination are crucial.
Related
Parabens or Preservatives: in your food and makeup
It is common to find the claim ‘parabens-free’ on a label these days. Such claims can be specifically found in some cosmetic products. The...
A2 Milk: Why you should know more about it?
You might have heard about A2 milk and the claims that it is better than the regular milk (A1 milk) commonly available in the market. Consumer...
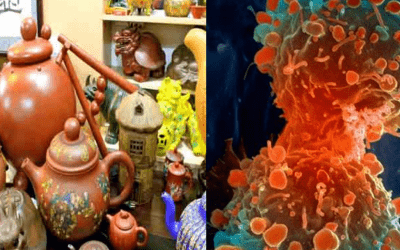
Ceramics in your home may cause cancer
The findings, led by the University of Plymouth in England, showed that cadmium ceramics wares and glass painting in your house might contain high...