Living Will becomes crucial since Passive Euthanasia is legal in India now
In March this year, in what was a landmark judgement, the highest court of the country allowed ‘peaceful death’ (passive euthanasia in medical terms) of terminally ill (vegetative state) patients when according to medical advice the patients are in ‘coma’ or in a state of condition where their chances of survival are considered ‘remote’. Alongside, it has made it mandatory to set strict guidelines that will govern when the same is permitted. The ‘living will’, therefore, becomes a crucial piece of document in this scenario.
Difference between Active Euthanasia and Passive euthanasia
Active euthanasia: The intentional act of causing the death of a patient in great suffering, is illegal in India and cannot be done. It entails deliberately causing the patient’s death through injections or overdose.
Passive euthanasia: the withdrawal of medical treatment with the deliberate intention to hasten a terminally ill patient’s death, is now allowed thanks to the recent SC judgement.
Here it must be mentioned that the Supreme Court also laid down guidelines for adoption of a living will, including who would execute it and how a nod for passive euthanasia would be granted by the Medical Board.
Claiming the Right to Die, Terminally ill patients can now make a living will
What is a Living Will?
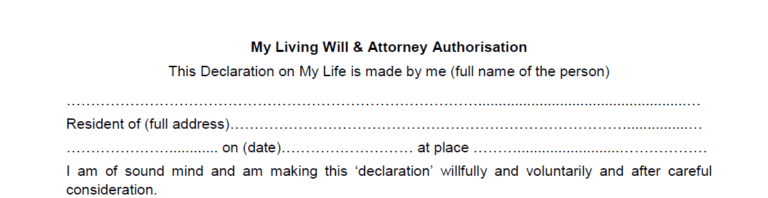
The ‘living will’ is an important document that a person, with deteriorating health or terminally ill, can execute in advance. Through this document, such a person can choose not to remain in a vegetative state with a life-support system. If that person comes into that state, and it will no longer be possible for him/her to express their wishes in spoken words, the document will be presented to hospital authorities for appropriate action. Thus, in a living will, a person can make a statement in advance that their life should not be prolonged by putting them on a ventilator or an artificial support system.
Why a Living Will?
So, here’s a document that will on the one hand help relatives who may not want to pull the plug (terminate the life-saving systems in place) till the doctors treating the patient feel that the patient’s situation is hopeless – in any case, it will help to relieve them of the ‘guilt’ feeling that they are opting to snap off the life-support systems for whatever reason, whether it’s to save money or time. On the other hand, it strengthens the position of doctors in cases concerning the terminally ill – since the patient has already executed the living will, the decision of the doctors to end life-support systems will not be seen to have been made under pressure of relatives, especially when a large amount of property is involved.
Living will may be used by a person to also outline a full range of treatment preferences. It can spell out a person’s preferences for tube-feeding, artificial hydration, and pain medication when he/she can no longer communicate his/her choices.
Side Notes: What Is Palliative Care?
World Health Organization describes palliative care as a multidisciplinary approach that improves the quality of life of patients with life-threatening illnesses, and their families by relieving suffering and pain—physical, psychological and spiritual.
Depending on the requirements, palliative-care services can be extended at three levels:
- Outpatient clinic (provide consultation, guidance and linking to homecare services)
- Home care (patient treated at home through paramedics, counselors, volunteers)
- Inpatient clinic (admitted to intensive and/or recovery care)
Connecting the Points
- Palliative care needs to be started at the very early stages of one’s disease.
- Doctors and patient need to be educated on alleviating suffering and pain.
- The old and the infirm having no will to live and not responding to treatment either, with the disease having reached a terminal stage, should be allowed to die in peace without further suffering and pain.
- The patient and the family may be informed about organ/tissue donation through National Organ and Tissue Transplant Organization (NOTTO) and Deceased Organ and Retrieval Organization (DOROSO).